olio for health plans
Scaling Efficient UM Teams for Health Plans
Rethink Utilization Management with Olio, ensuring quality outcomes and cost-efficiency through real-time member co-management across all care settings and providers.
Olio Delivers Proven Value & Results
Unlock Tangible Savings and Improved Care with Streamlined Patient Co-Management
97%
Average percentage of Olio post-acute users who use Olio in their workflow every day
<60 Min
Olio clients receive post-acute response times of less than 1 hour, compared to the avg. 24-48 hours
60 Days
We can successfully launch most markets in 60 days with our proven process
1:160
One user at a midwest physician group co-managing 160 skilled nursing facilities
Simplify the Complexity of Utilization Management Across Care Settings
Health plans face an array of challenges that hinder efficiency, elevate costs, and compromise outcomes — not least of which is the ability to co-manage members across care settings.
- QEnsuring line of sight into post-acute care, home health, and additional care settings
- QKnowing who is on your members’ care teams & how to reach them
- QMeasuring engagement and responsiveness effort with your member co-management partners
- QStandardizing processes and workflows that scale
- QElevating care teams across the network in an accountable member co-management ecosystem
- QReducing unnecessary administrative time and burden for your teams and providers
- QReducing cost of care without compromising member outcomes
Transform Obstacles into Opportunities with Olio
Improve performance, boost revenue growth, and scale operational efficiencies with a unified solution that gives the same access, visibility, and workflows to all stakeholders.
Optimize Utilization Management
Ensure the right care is given at the right time and place with enhanced communication and collaboration.
Measure & Enhance Network Performance
Track network efficacy & set strategy to course-correct with real-time clinical insights and rolling performance metrics by business line and provider group.
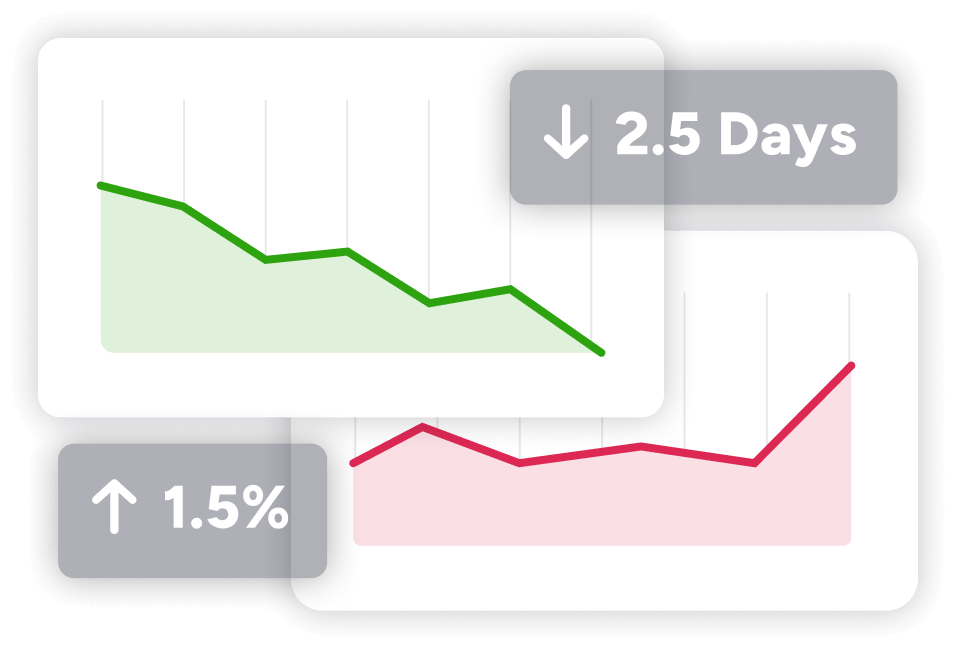
Significantly Impact the Total Cost of Care with Olio
Directly influence the total cost of care within all lines of business at the health plan with enhanced, streamlined UM functions across all care settings.
4 – 7x ROI
Experience an average 4-7x return on investment with Olio
Streamline Utilization Management with Olio
Compliance & Documentation
Ensure adherence to essential documentation and compliance norms with all stakeholders through a single source of truth.
Operational Efficiencies
Save time and maximize the capabilities of your UM teams and the care teams with which you co-manage members through a single, unified solution.
55 Hours
Saved across 15k+ lives
Easily Co-Manage Members Across All Your Lines of Business
Streamlined Processes
Streamline UM workflows, including initial and concurrent reviews, for any health plan to co-manage members across care settings.
Improved Connectivity
Gain a clearer line of sight into various care settings, ensuring optimal resource allocation and reduced readmissions.
Insight-Driven Decision Making
Eliminate delayed decision-making on behalf of your members and overcome operational challenges with real-time, accurate data.
Efficient Workflows
Create scalable workflows with the assurance of timely, accurate information available to all stakeholders.
Secure, Compliant Solutions
Share discrete data without compromising compliance using Olio’s purpose-built solution.
Clear ROI & Savings
See tangible ROI while driving savings and internal alignment.

55
administrative hours saved per week for their 15K member D-SNP population
PRESS RELEASE
Olio’s Patient Co-Management Solution a ‘Game Changer’ for Banner Health
Banner Health Plans turned to Olio to improve patient care and streamline processes with post-acute partners, resulting in lowered readmission rates that are ‘almost unheard of’.