Hypesmith CEO, Peggy Johnson, sat down with Olio to discuss the Center for Medicare and Medicaid Innovation (CMMI) goal of moving all Medicare and Medicaid lives to some form of total cost of care arrangement by 2030 and how Olio is supporting the initiative.
Overview
The Center for Medicare and Medicaid Innovation (CMMI) put out a white paper announcing in Q4 2021 their goal of serving all Medicare and Medicaid beneficiaries through accountable care or some form of total cost of care arrangement by 2030. Healthcare leaders understand that value over volume continues to be our nation’s best chance at affordability and have a strategic plant to transition a higher percentage of their business into risk arrangements. The challenge is identifying which strategies have resulted in the most significant impact and figuring out how to scale those efforts across a growing population.
Question:
You have been working with accountable care organizations for several years. Please explain progress that has been made in the shift from volume to value healthcare reimbursement?

There has been good progress made and we see ACO leaders focused on the shift. Most of progress has been in upside risk or shared savings and there hasn’t been the same progress on downside risk arrangements. The largest percentage of the Medicare and Medicaid population is still not in a managed environment, so fee for service is still dominant in the industry. NAACOs just released an article on the status of ACO participation in 2022. Total participation is still down from a peak of 561 participants in 2018. Much of that is due to changes within the program that are driving more organizations to downside risk. I think this highlights there is still a lot of work left to be done if CMMI wants to hit their 2030 targets.
Question:
What should ACO leaders do next to drive the shift from volume to value-based healthcare?
I’d broaden the question to include value-based care or population health as a whole, and I’ll explain why in a minute. In saying that, there are 3 must haves to successfully shift from volume to value-based care:
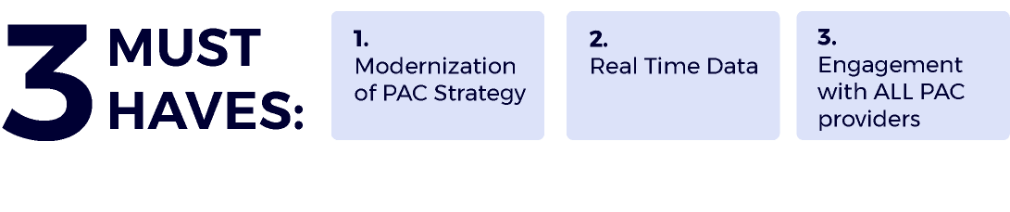
1. Modernize population health and post-acute care (PAC) strategies: Right now there is a heavy reliance on care coordinators to try and manage patients in the PAC space and interact with PAC providers. The problem is many of those methods center around outdated methods of communication and PAC management. It’s a resource heavy model that requires the addition of more people resources as volume increases. This isn’t a scalable solution in the long-term. A better, modern, approach involves providing PAC providers with technology support that makes them a valuable asset to your team and allows care coordinators to cover a larger percentage of patients.
2. Real time data: The volume of data generated within the healthcare industry is expanding exponentially, so getting a handle on data overload and getting access to the right data quickly to make strategic decisions is key. The industry can’t wait around for claims data that is so old by the time you get it, many opportunities for improvement have passed. For population health leaders to understand how PAC providers are caring for their patients, they must be able to consistently review things in real time like rates of readmission, ED visits, length of stay, PAC provider quality of care and engagement. Having easy, real-time, access to these things allows a course of action to be set for PACs who are not performing or engaging.
3. Engagement of All PAC Providers: We recently analyzed ACO performance data over the past 5 years and noticed some interesting trends. Those that generated earning savings, on average, had a lower skilled nursing spend per beneficiary than those that did not generate savings. This is to be expected, typically as cost decreases savings increase. The surprising trend was ACO’s that generated savings had a HIGHER cost per beneficiary for in-patient rehab and home health. I think this highlights how important PAC engagement is across the spectrum and not solely focused on skilled nursing utilization. Most PAC management strategies revolve around managing the skilled environment, for a defined narrow network. Over the next 3 years it’s going to be critical for organizations to get a better handle on all levels of post-acute care and how to manage outcomes for providers outside their narrow network.
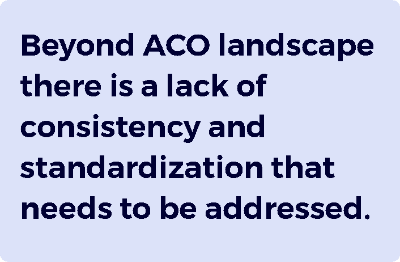
I mentioned previously we view the shift to value beyond just the ACO landscape. One area of future concern I see for a lot of organizations is having separate internal strategies for different patient populations. One group may be focused on ACO performance, while another is managing bundled payments, owned health plans, Medicare Advantage lives, etc. There is a lack of consistency and standardization that needs to be addressed if the CMMI goal is to become of reality by 2030.
The solution to better outcomes at lower costs really relies on the population health and post-acute provider landscape to be engaged and incentivized to keep patients healthier.
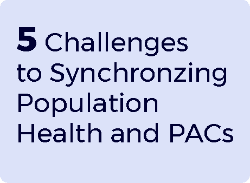
Population Health’s 5 main challenges when transitioning patients to post-acute care include:
- They have no visibility into home health and other transitional care
- They lack information after a patient discharges from skilled nursing
- There is no access to patient data after a patient transfers
- They get no warning from PAC providers prior to a patient being readmitted, and
- There is no engagement or data from PAC providers outside of existing
Technology that addresses ACOs main concerns of synchronization between population health and all post-acute care providers has been missing. Everyone needs to be on the same team with the same view to move into more successful patient outcomes.
Question:
So how is Olio helping overcome these challenges?
Our application gets everyone on the same team, which means allowing post-acute providers to actually be a part of the team, really for the first time. Population health teams can operationalize their PAC engagement and workflow process and access data when they need it to make strategic decisions quickly. Our clients have used Olio to deploy PAC management strategies that are built for value-based care success. It boils down to 5 simple abilities:
- Adoptability – It must be easy for PAC providers to execute
- Visibility – Insight into all levels of post-acute care
- Scalability – Engagement with providers beyond a narrow network
- Accountability – Realtime data to measure performance
- Affordability – Reducing total cost of care, not shifting expenses from one area of spend to another

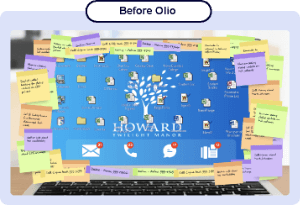
Before Olio, our clients were making significant investments in people and tech resources every year to coordinate with a handful of PAC providers, and the number was on a trajectory to grow as they hired more and more care coordinators. Once they start using our software, they gain efficiencies for care coordinators and can engage PAC providers outside of a narrow network to improve engagement on patient care without having to add more staff.
Too often, in the rush to make a difference and take on risk, organizations will implement things without a full appreciation of the complexities of what is happening or an understanding of why things are structured the way they are. Having data to understand what is happening allows informed changes.
In addition to operationalizing PAC workflows and making everyone’s life less complicated, Our application shares real time data in a user-friendly manner on readmission rates, length of stay and engagement by PAC. That is key to their short term and long-term strategy decisions. Basically, before Olio our clients were waiting for claims data as well as returned calls, emails, voicemails etc. Now they have instant access to resources and data.
Question:
When you work with your ACO clients, do you see resistance from the PACs that are not in their network?
When we reach out to the PACs, in or out of a preferred network, they are ecstatic for relief. They want to do the right thing for patients and be an active member of the team. They are just as much invested in operational efficiencies through synchronization of population health.
The PAC sector has seen its most profound challenges from deadly COVID-19 outbreaks in skilled nursing facilities (SNFs) to a suddenly accelerated need for the services provided by home health and hospice. They are consistently bombarded with phone calls, voice mails, emails, text messages, instant messaging, and personal visits from care coordinators – prior to Olio there was no simplified way to coordinate. It is very simple for them to engage with our platform. Its user friendly and accessible through mobile devices. Everyone is familiar with the modern way of communicating these days and it is much easier for them to grab their cell phone and enter a quick escalation than play phone or email tag.
PACs know everyone needs to be on the same team with the same view as they move into 2022. It is also very valuable to them that we do not charge PACs for the software.
Question:
What are some of the key results you are most proud of since Olio entered the market in 2015?
To start with we have had 100% client retention and expansion. Once our clients start with Olio, they expand to other populations and continue to request additional services, so we are very proud of that.

Also, we are already working with some of the leaders in value-based arrangements including Optum, Village MD, Banner Health, and Indiana University Hospital System – just to name a few. All our clients are seeing readmission and length of stay reductions, an increasing number of PAC relationships and engagement, and scalability so care coordinators get needed relief.
It feels great to be part of the successful transition from volume to value-based care. We all want affordability in our health care system, and the Olio team is proud to do our part.
Interview Summary
Elderly patients covered by Medicare are regarded as the greatest financial drain on the health-care system. It is a growing population that requires special attention and communication. The existing operational processes and EMRs fail to connect the dots between population health and post-acute care.
There is a growing demand for PAC services with the aging population, and there is a scarcity of ACO organizational resources needed to optimize the PAC referral / coordination processes. Based on these factors and the CMMI goals for 2030 ACO leaders, hospital decision-makers, and PAC stakeholders are recognizing they need to find right tools and capture the right data to team up and improve outcomes and lower cost.
Effective risk sharing requires a coordinated-system centered on reducing hassles and improving outcomes for patients rather than simply cutting costs. Population health and post-acute teams can work together, continually sharing information and insights about their mutual patients and providing services needed to keep those patients in the best possible health.
The daily discipline of measuring post-acute provider engagement, length of stay, and readmissions at all PACs in real time and having an easy way to collaborate is the most effective way to enhance the value of care. With Olio, clients have become more successful at all these things.